Anterior Lumbar Interbody Fusion (ALIF) surgery is a common treatment for back or leg pain caused by degenerative disc disease. When degeneration occurs, the discs may begin to bulge out or rupture. This can lead to compression of the spinal nerves or cause inflammation in the surrounding vertebral joints. ALIF can also be used to treat nerve compression, disc space collapse, scoliosis, and other conditions.Surgery is usually considered only after conservative therapies have failed to successfully treat back pain and sciatica (leg pain).
An anterior approach maybe recommended for a number of reasons, including:
An ALIF may be done alone or in conjunction with another spinal fusion approach depending on your particular condition.
In this surgical procedure your lumbar spine is accessed from the front, as opposed to other interbody fusions, which may enter from the side or back of the body. This requires the involvement of a vascular surgeon to provide access to the spine. Major blood vessels such as the aorta and vena cava will need to be retracted to get a clear view of the front of the spine and the expertise of a vascular surgeon ensures this is done safely.Most of the lumbar disc is removed from in between two adjacent vertebrae in the lumbar spine. These vertebrae are then fused (joined) together using an implant filled with a bone graft substitute. Fusion surgeries typically require the use of bone graft to facilitate fusion. The bone graft material works as a bridge or platform that binds or fuses two vertebrae together and promotes new bone formation. This stimulates the growth of a solid mass of bone, and helps in stabilising the spine. This bone graft, along with intervertebral cage (synthetic implants), will take the place of the intervertebral disc, which is almost entirely removed in the process.
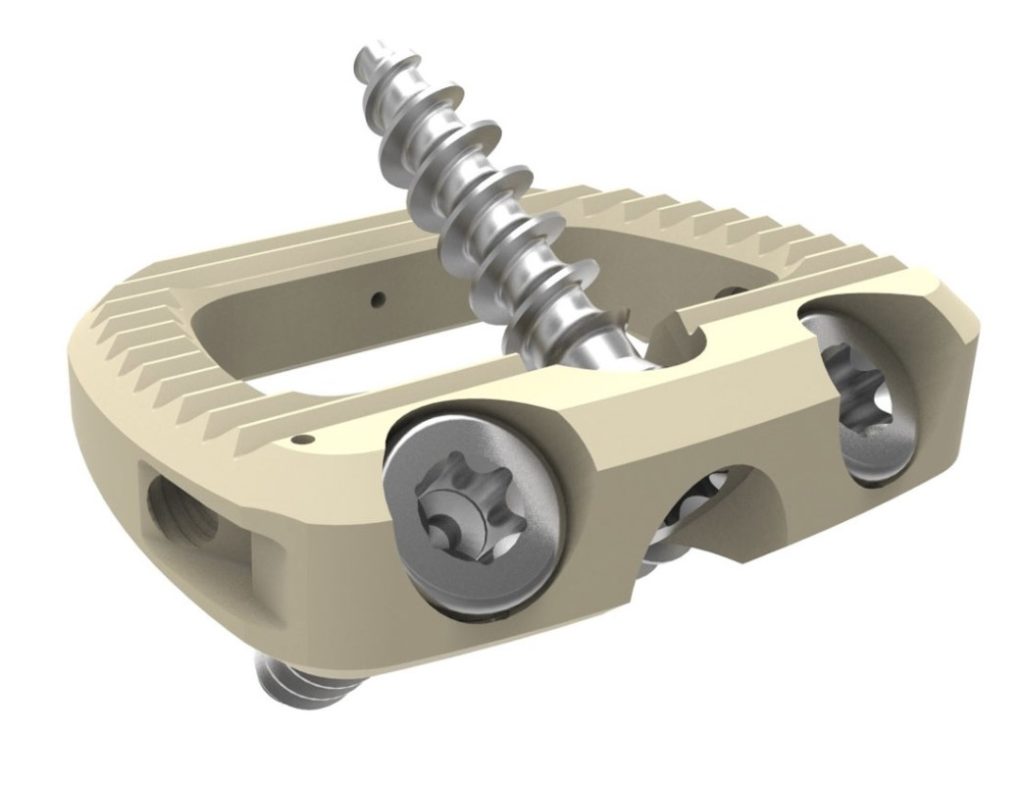

You will be given a general anaesthetic to put you to sleep. A breathing tube (endotracheal tube) will be inserted and you will be given a dose of antibiotics to help prevent infection. You will have an indwelling catheter (IDC) placed to help you pass urine during and after surgery. You will be placed on your back on the operating table and calf compression devices will be attached to your legs. This helps to minimise the risk of developing blood clots in your legs. An X-ray will be taken to identify and mark the level of the spine requiring surgery. The vascular surgeon makes a small incision in the abdomen and gently pushes and retracts the abdominal contents (intestine, ureters, iliac arteries and veins) to the side. Once access has been provided, the neurosurgeon takes over and the damaged disc will be removed. Once the disc space has been cleared out, the implant will be inserted between the two adjoining vertebrae. This implant or cage contains bone graft material, which promotes bone healing and facilitates the fusion. The implant restores the height between the vertebrae and once fused, provides stability, and length to the lumbar spine, while also relieving the symptoms of pain and inflammation. Once complete, imaging is used again to confirm the placement of the implant. The retractors are then withdrawn, layers are sutured and the skin is closed using staples. A dressing is applied.
Patients are allowed to mobilise the day after surgery is performed, and have a Patient Controlled Analgesia (PCA) device to help manage your pain. A postoperative CT is usually performed to verify position of the implant. You are usually in hospital for approximately 3-4 days prior to discharge home, or if required to a rehabilitation unit. It is usual to feel some pain after surgery, especially at the incision site. This should decrease a little each day. You will be discharged with pain relief medications to manage this, and given a booklet outlining all postoperative instructions. Once at home you will receive a follow up phone call from the practice nurse. Postoperative appointments will be arranged for you at both the 2 and 6 week mark with the practice nurse and Dr Winder respectively.
Once home, frequent short walks are recommended. This will help in your recovery and also reduces the risk of blood clots forming in your legs. A gradual increase in physical activity is advised.
You must not lift anything heavier than 5kg for the first 6 weeks post-operatively and avoid twisting and bending movements. If bending is necessary, you must bend using your knees and not your back.
Avoid housework such as vacuuming, mowing and hanging washing on the line for the first 6 weeks postoperatively.
Sitting may be the most uncomfortable position postoperatively and should be restricted to 30 minutes at a time in the first week after surgery. You may gradually increase the time in small increments, as you are able.
You may drive 1 week after surgery if you are comfortable to do so but avoid long distances. If you do need to travel for longer periods them make sure you stop and take frequent breaks.
Physiotherapy is recommended 2 to 3 weeks after your surgery. Gentle stretches and core stability exercises will help to strengthen your back after surgery.
Keep your wound dry, you will be given extra waterproof dressings on discharge. Your staples should be removed between 7-10 days after surgery. This can be done by making an appointment with your GP or Dr Winder’s practice nurse. You may shower as normal but if your dressing becomes waterlogged it should be changed. Dr Winder’s practice nurse will check your wound at your 2 weeks postoperative appointment.
Dr Winder will discuss resuming sports and other physical activity at your 6 weeks appointment
Please note that it is not uncommon to have localised back stiffness for up to 6 weeks. This will generally resolve gradually.
Depending on the degree of nerve compression, it is also very common to have some degree of leg discomfort or numbness, as it will take time for the compressed nerve to recover. Please do not be alarmed if you have some intermittent pain in the legs as this is a normal part of the healing process.It is usual to feel some pain after surgery, especially at the incision site.
Some of the possible complications for anterior spine surgery include:
If you require surgery, Dr Winder will discuss all relevant risks during your consultation.
There are risks associated with any surgery, the most common being:
A full medical history including allergies, medical conditions and previous surgery is required before your surgery to help reduce the risk of complications occurring.
Please make sure you bring your scans either on film or on CD on the day of surgery, and inform Dr Winder or his team if you are taking any blood thinners such as aspirin, clopidogrel, warfarin or apixaban.